
Mechanisms and consequences
Albumin and thyroxine, either separately or together, are important contributors to most of our physiological functions. Albumin carries about 10% of the thyroid hormone thyroxine. Binding of thyroxine to albumin is managed allosterically which means changes elsewhere on albumin structure can alter its thyroxine-carrying capacity.
Thyroxine is both produced naturally and can be administered therapeutically. It binds to five sites on albumin, being Tr-1, Tr-2, Tr-3, Tr-4 and Tr-5. These partially overlap the Fatty Acid (FA) binding sites FA3-4, FA5, FA7, FA9. Thyroxine’s primary binding site on albumin is currently disputed with various authors claiming each of the various sites.
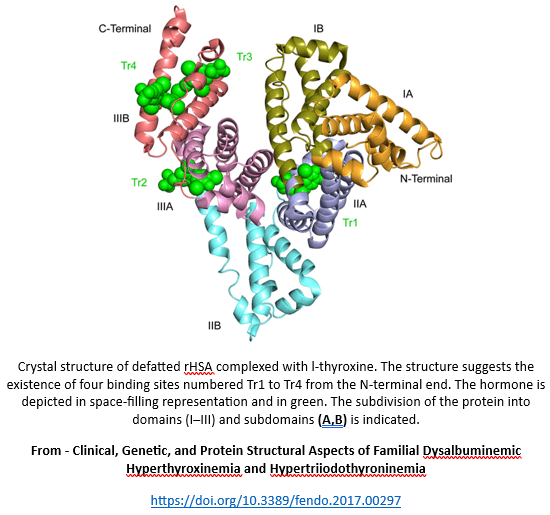
Thyroxine binding sites
Thyroxine site
FA sites
Comments
Tr-1
Subdomain IIA; FA7, Sudlow site 1 *
Trp214 (IIA), Arg218 (IIA) and Arg 222 (IIA) are not affected by thyroxine binding to Tr-1.
Tr-2
Subdomain IIIA; FA3-4, Sudlow site II *
FA3 - binds fatty acids –
- linearly - ≤ 12–14 carbons,
- folded ≥ 12–14 carbons.
The folding of long chain PUFAs may be a functional prerequisite.Tr-3
Subdomain IIIB; FA5
Binds up to two thyroxine molecules.
Tr-4
Subdomain IIIB; FA5
Binds up to two thyroxine molecules.
Tr-5
Between domains I + III i.e. FA9
A high-affinity site for thyroxine in the presence of excess fatty acid.One mol albumin typically carries 1–2 mol FAs. An increased quantity is required to stimulate the structural changes necessary to create Tr-5 site.
* Confusion seems to exist regarding FA7 and Sudlow Site 1, and FA3-4 and Sudlow Site 2. Some authors use both terms interchangeably whilst others maintain separate sites with significant overlap.
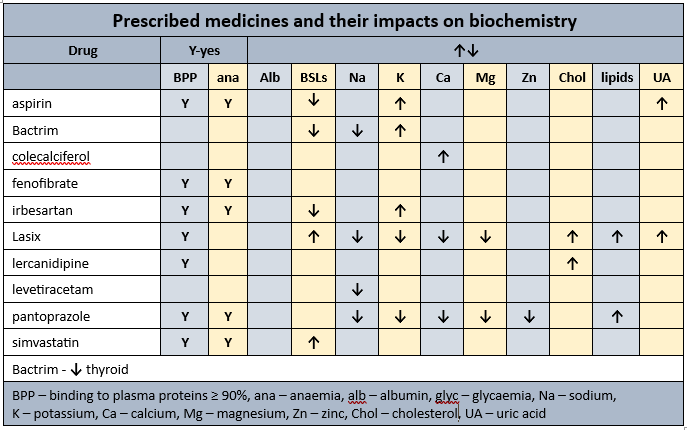
Glycation
An inverse correlation seems to exist between degree of glycation and fatty acid binding affinity. As the degree of glycation increases, so the binding affinities of fatty acids change. Initial evidence indicates 3 sites (FA2, FA4, FA5) retain high affinity whilst other sites assume low affinity. Glycation can therefore indirectly alter thyroxine’s binding capacity to albumin through FA4 and FA5.
Fatty Acids
Fatty acids compete with thyroxine for binding at all its sites, and also –
- inhibit the binding of thyroxine if the fatty acid:albumin ratio is high,
- induce structural changes to albumin eg creation of a fifth thyroxine binding site,
- alter albumin’s capacity to carry thyroxine.
Thyroxine binding sites
Subdomain
Thyroxine binding sites.
IA
IB
IIA
Tr-1
IIB
IIIA
Tr-2
IIIB
Tr-3, Tr-4
Domains I + II interface
Tr-5
Clinical concerns
The research seems to still be at the “what is going on” stage, and has not yet reached the “what can we do about it nutritionally” stage.
Clinical Questions
What actions will you initiate as you a review a person who is prescribed one or more drugs that utilize albumin as a carrier -
- will you clarify and monitor thyroid function?
- if thyroid function is altered, will you question whether a contributing factor could be some of the prescribed medicines altering albumin’s capacity to carry thyroxine?
Conclusions
Albumin and thyroxine are important in maintaining body function, and are negatively impacted both directly and indirectly, by prescribed medicines.
Case study
The comments refer to the drug-nutrient, drug-food, and PharmacoNutrition effects only.
Data summary
Medical history with nutritional aspect
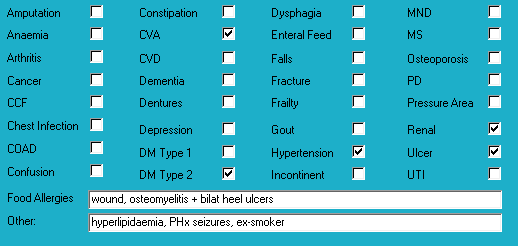
Biochemistry with nutritional aspect
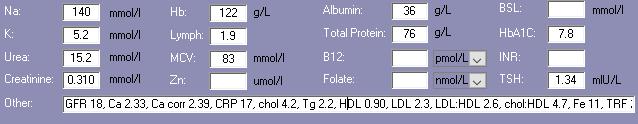
Prescribed medications side effects profile - biochemistry
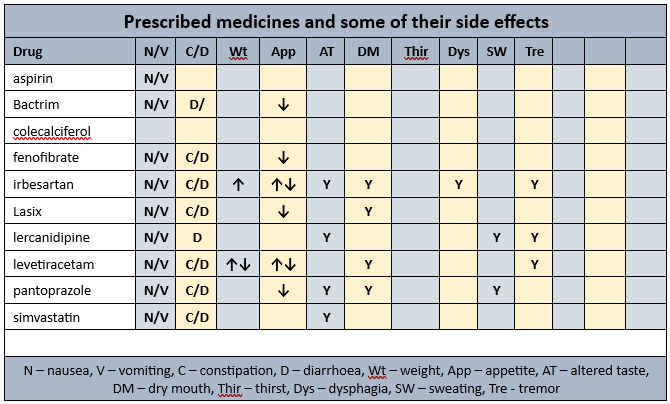
Prescribed medications side effects profile
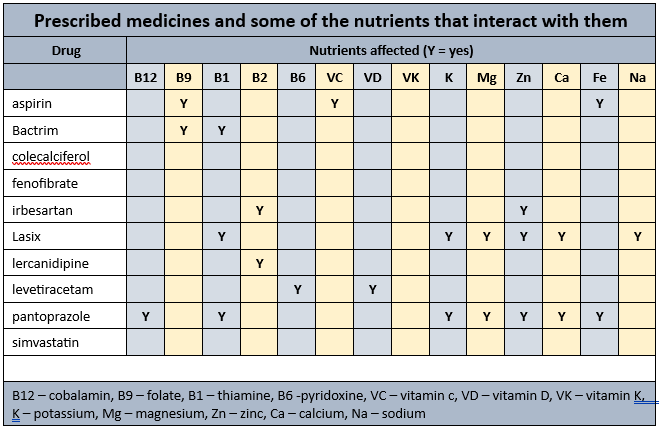
Prescribed medications affected nutrients profile
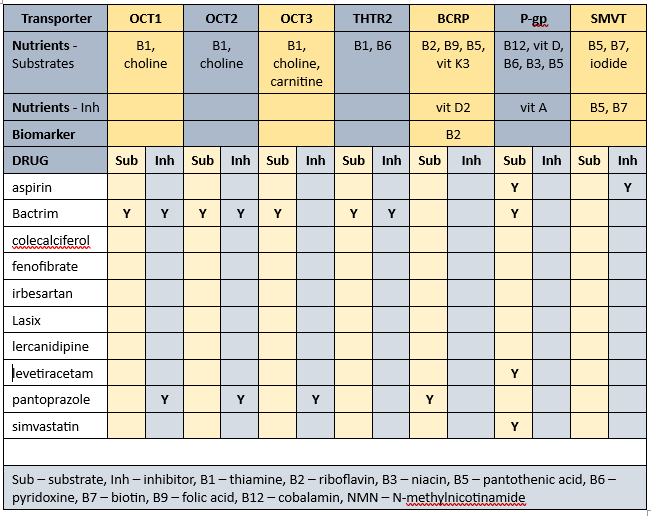
Transporter-mediated interactions and nutrients matrix 1
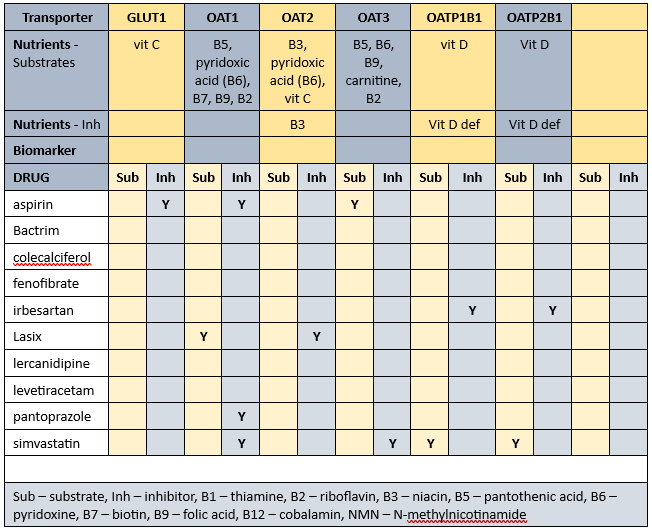
Transporter-mediated interactions and nutrients matrix 2
Biochemistry
Recent relevant results within acceptable ranges.
Glycaemia
BSLs (Jan)
- before breakfast - 7.4-13.3; recommended range 4-6
- daily range - 5.3-16.1; recommended range 4-10
- reportable limits: < 3 and > 20
- checked daily tds
- recent HbA1c indicates acceptable overall glycaemic control
Diabetes drugs
- novomix has a time to onset of 5-15 minutes, variable time to peak, and duration of 10-16 hours
- novomix 30 110U mane, 50U midday, 30U nocte
Diabetes drugs coverage
- before breakfast BSLs - minimal, if any, coverage from previous morning's novomix 30 or previous midday's novomix 30, possibly some coverage from previous evening's novomix 30
- before midday BSLs - minimal, if any, coverage from previous midday's novomix 30 or previous evenings novomix 30; covered by current morning's novomix 30
- before evening meal BSLs - minimal, if any, coverage from previous evening's novomix 30; covered by current morning's novomix 30 and current midday's novomix 30.
Currently prescribed 5 medications that alter glycaemia.
PharmacoNutrition
Aspirin
Caffeine increases aspirin absorption.
Aspirin reversibly decreases gastric vitamin C levels.
Aspirin plus vitamin C (960 mg/day) attenuates drug-induced gastric damage and restores anti-oxidant protection.
Aspirin inhibits vitamin C absorption by either inhibiting vitamin C binding to albumin, or by inhibiting/regulating/modulating GLUT1 (glucose transporter 1) uptake of vitamin C as DHA (dehydroascorbic acid).
If there is concurrent administration of a vitamin C intervention and aspirin then advisable to administer vitamin C prior to drug as vitamin C does not impact drug absorption whereas the drug does impact vitamin C’s absorption.
Aspirin has a negative impact on folate status - the mechanism of action remains speculative.
Bactrim
Folic acid supplement advisable if long term Bactrim use.
Bactrim associated with thiamine deficiency.
Recommendation for regular monitoring of electrolytes, especially sodium, and for hyperkalaemia to be managed aggressively, especially if Bactrim administered to elderly with underlying renal dysfunction.
Colecalciferol
Coffee inhibits vitamin D uptake by inhibiting the osteoblasts (bone builders) vitamin D receptors, consequently decreasing calcium and zinc absorption.
Furosemide
Frusemide increases urinary excretion of calcium, magnesium, potassium, sodium and thiamine.
Dose-dependent furosemide causation of thiamine deficiency due to increased urinary excretion (of thiamine) related to urine flow rate.
Elevated fatty acid levels significantly decrease frusemide binding to albumin - this has potential clinical implications in those with hyperlipidaemia.
Pantoprazole
Pantoprazole decreases B12, vitamin C, magnesium, zinc and iron absorption, may decrease calcium absorption, and decreases thiamine availability.
Statins
Statins interfere early in the cholesterol metabolic pathway and consequently decrease -
- conversion of sun to vitamin D - vitamin D intervention recommended;
- production of CoQ10 - important in cellular energy production; CoQ10 intervention recommended;
- DHEA production - low DHEA associated with increased risk of metabolic syndrome; intervention recommended.
Lipid levels are well within acceptable range therefore advisable to review necessity for its continued prescription especially since there is acceptable glycaemic control. There is variability between pathology laboratories with regard to appropriate lower acceptable cholesterol level - some pathology ranges have set the lower acceptable limit at 3.5, others 3.0, and some do not set a lower limit. Cholesterol is important in brain structure and function amongst many other roles.
Mr ADO is prescribed 3 medicines that alter lipid status.
Daily doubles
Currently prescribed the daily double ie 2 drugs that decrease thiamine availability, being frusemide and pantoprazole. Thiamine is important in glycaemic control therefore advisable to clarify thiamine status and adequacy of dietary thiamine intake. If Diet History shows very good thiamine intake, therefore if blood test results indicate low thiamine status then a drug-nutrient-transporter interaction is likely influencing thiamine availability by inhibiting some of the relevant transporters.
Currently prescribed the daily double ie two drugs decrease magnesium availability - being frusemide and pantoprazole. Magnesium deficiency manifests as confusion, disorientation, personality changes, loss of appetite, depression, muscle cramps, tingling, numbness, hypertension, cardiac dysrhythmia, seizures. Magnesium is an intracellular ion therefore serum levels are unlikely to detect early depletion of status. Cellular magnesium status remains unknown whilst magnesium levels within acceptable range however if magnesium levels are low then that typically indicates significant cellular depletion and intervention recommended.
Membrane transporters
Prescribed medications can alter the functionality of membrane transporters and consequently the nutrients they carry. Nutrients impacted by Mr ADO’s prescribed medications -affected transporters include -
- substrates – thiamine, riboflavin, niacin, pantothenate, pyridoxine, biotin, folate, B12, vitamin C, vitamin D, vitamin K3, choline, carnitine, iodide;
- inhibitors – niacin, pantothenate, biotin, vitamin D, vitamin A.
The duration of drug inhibition of transporters currently remains unknown.
Bowel management
- no regular intervention prescribed;
- no PRN interventions prescribed;
- no Nurse Initiated interventions administered.
Staff comments
Staff advise Mr ADO eats well, makes good food choices, no food refusals, and really enjoys the desserts.
Observations
Mr ADO is a man of size who was sitting in his room waiting for his dressings to be attended to. He told me he does not feel upset in the tummy, nor does he spend much time outside when its hot, and sleeps well
Mr ADO has remained remarkably stable about 125 kg for the last 7 months.
PharmacoNutrition comments
Wound healing
Mr ADO has a wound - nutritional interventions that support to wound healing include -
- ensure adequate status of B12, magnesium, zinc and iron - pantoprazole is prescribed which compromises their status;
- adequate vitamin D status - evidence indicates low vitamin D status is associated with delayed wound healing. Currently prescribed levetiracetam which decreases vitamin D availability, and a vitamin D intervention. Advisable to monitor vitamin D status on a regular basis whilst wound is healing.
Vitamin C is important in collagen formation and the strength of the collagen; the proton pump inhibitors reduce availability of active vitamin C. It is likely wound healing will be delayed, and of poor quality whilst there is reduced availability of active vitamin C. It is also likely vitamin C interventions are unlikely to be effective whilst a proton pump inhibitor is prescribed.
Mr ADO is in the difficult position of being prescribed a proton pump inhibitor and having a wound that is unlikely to heal properly whilst a proton pump inhibitor is prescribed. Advisable to consider -
- whether proton pump inhibitor prescription is still required;
- if suppression of gastric acidity is still required then could it be managed with an H2 antagonist such as ranitidine (there is a general belief that they cause less nutritional harm than proton pump inhibitors);
- if the proton pump inhibitor intervention can be ceased until the wound is healed.
Insulin resistance
There are a number of nutritional interventions to improve insulin sensitivity or reduce insulin resistance including -
- vitamin D within acceptable range - early evidence indicates low vitamin D is a predictor of peripheral insulin resistance and elevated inflammatory response markers. Currently prescribed levetiracetam which decreases vitamin D availability, and a vitamin D intervention. Advisable to monitor vitamin D status on a regular basis whilst wound is healing;
- magnesium – is important in glycaemic control and inadequate intake may impair insulin synthesis, secretion and signalling pathways; in fact there is evidence of an inverse correlation between magnesium status and diabetes incidence. Currently prescribed Lasix and pantoprazole which significantly decrease magnesium availability, and currently no intervention. Advisable to monitor status on a regular basis;
- chromium - evidence indicates chromium both increases the number of insulin receptor cells on cell walls, and improves intracellular response to insulin. Mr ADO may benefit from a short term (90-120 days) intervention of elemental chromium;
- thiamine - people with diabetes have a significantly increased urinary excretion of thiamine; thiamine is important in glycaemic control. Currently prescribed Bactrim, Lasix and pantoprazole, all of which impair thiamine availability. If Diet History shows very good thiamine intake, and if blood test results indicate low thiamine status, then a drug-nutrient-transporter interaction is likely influencing thiamine availability by inhibiting some of the relevant transporters. A thiamine intervention is unlikely to confer benefit if there is drug-induced inhibition of relevant transporter(s).
- TNF-α – evidence indicates TNF- α has systemic effects that result in insulin resistance and NIDDM; low B12 status exacerbates elevated TNF- α. Currently prescribed pantoprazole which decreases B12 absorption therefore advisable to monitor B12 status on a regular basis;
- zinc – is integral to insulin formation, and enhances insulin sensitivity through stimulation of insulin receptors; inadequate intake may impair insulin synthesis, secretion and signalling pathways. It is important in the glucose metabolism, protects the mitochondria from oxidative stress and glycation, and altered glomerular function, as well as modifying the inflammatory response pathway and activation of the polyol pathway (a part of intracellular signalling and metabolism). Currently prescribed irbesartan, Lasix, and pantoprazole therefore advisable to monitor zinc status on a regular basis;
- potassium - important in the glucose metabolism, and functions in β-cells; inadequate intake may impair insulin synthesis, secretion and signalling pathways. Currently prescribed Lasix and pantoprazole which reduce potassium availability;
- calcium - important in the glucose metabolism, and functions in β-cells; inadequate intake may impair insulin synthesis, secretion and signalling pathways. Currently prescribed Lasix and pantoprazole which reduce potassium availability;
PPI prescription
Mr ADO has been prescribed a PPI since admission ie 19 months ago, and probably before then. The evidence is increasing that proton pump inhibitors such as pantoprazole significantly impair magnesium absorption. Magnesium deficiency manifests as confusion, disorientation, personality changes, loss of appetite, depression, muscle cramps, tingling, numbness, hypertension, cardiac dysrhythmia, seizures, decreased absorption of thiamine, vitamin C, vitamin D and iodine. Magnesium is an intracellular ion therefore serum levels are unlikely to detect early depletion of status, however if magnesium levels are low then typically indicates significant cellular depletion and intervention recommended.
Men require 420 mg magnesium per day, however there are side effects from magnesium interventions that provide 350+ mg elemental magnesium/day from non-food sources.
Currently prescribed Lasix and pantoprazole which significantly decrease magnesium availability. Advisable to check magnesium levels and if still marginal then review current magnesium management strategy and consider an intervention that provides about 300 mg elemental magnesium per day.
What else would you include?
Please read this as it is important …
The information in this article is provided to support Health Professionals. It is not an exhaustive protocol and Health Professionals are advised that adequate professional supervision is accessed to ensure that Duty of Care obligations with respect to safe administration of medicines is met for each consumer.

