
Mechanisms and consequences
Albumin and minerals in combination encompass a broad range of physiological. Albumin’s multiple metal binding sites enables it to carry key minerals such as calcium, cobalt, copper, manganese, magnesium, selenium, zinc.
The importance of zinc
The interdependence of albumin and insulin is regulated by zinc availability. Zinc is important in the production and availability of insulin, and its release from insulin enables insulin activation. The released zinc then attaches to albumin – and albumin’s capacity to bind zinc regulates the availability of active insulin. Further, insulin levels directly affect albumin synthesis ie low insulin levels cause reduced albumin synthesis and vice versa.
Non-esterified fatty acids (NEFAs) encompass both saturated and unsaturated forms. NEFAs are also transported by albumin, and their binding to FA2 (Fatty Acid 2 site) triggers albumin to release zinc. As NEFA levels increase so albumin’s capacity to bind zinc diminishes resulting in reduced availability of activated insulin.
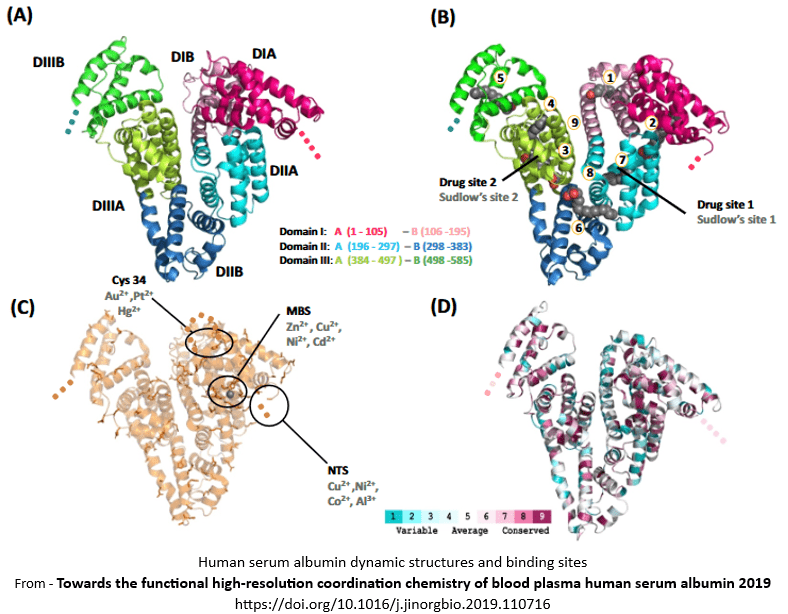
Binding Sites
Albumin’s capacity to bind minerals is based on 7 amino acids that are located within 4 binding sites.
The 7 amino acids are arginine (Arg), aspartic acid (Asp), cysteine (Cys), glutamic acid (Glu), histidine (His), lysine (Lys), tryptophan (Trp) and are commonly called “residues”.
The 4 four metal binding sites are –
1. Site A - aka Multi-metal Binding Site A or MBS-A or Cadmium site A
Located at the domain I/II interface with residues from both domains involved in the interactions.
Site A's location also overlaps with the FA2 site. Binding on one site may alter binding capability on the other site.
Involves His67, Asn99, His247, and Asp249 residues.
2. Site B - aka Multi-metal Binding Site B or MBS-B or Cadmium site B
May also be an inter-domain site however its location and details are currently indeterminate.
3. NTS - aka N-terminal binding site, or ‘ATCUN’ (Amino Terminal Copper and Nickel binding site)
Located in subdomain IA at the N-terminus.
Involves Asp1, Ala2, and His3 residues.
4. Cys-34
Located in subdomain IA.
Binds gold, mercury and platinum ions.
Albumin’s metal binding sites
Distribution of minerals and their binding sites
Table of minerals and their known binding sites on albumin
Calcium
Subdomain IIA – Asp-249,
Sites A + B.Chloride
Status unknown for chloride ions.
Chromium
Location indeterminate.
Cobalt
Site B – primary,
His-9, His-67;
Site A – secondary,
His-9, His-67;
NTS;
Cys-34 – does not bind cobalt.Copper
NTS – primary,
Subdomain IA - Asp1-Ala2-His3. His-3 is considered essential;
Site-A – secondary,
Interdomain I/II interface, surrounded by FA1, FA2, and FA7 binding sites.Fluoride
Status unknown for fluoride ions.
Iodine
Status unknown for fluoride ions.
Iron
Haem complex - subdomain IB,
Tyr138, Tyr161, and FA1.Magnesium
Domain II – Asp-249,
Sites A + B.Manganese
Site B – primary;
Site A – secondary.Molybdenum
Location currently indeterminate.
Potassium
No evidence of carriage by albumin.
Selenium
Cys34 – subdomain IA;
Assumed binding site for selenium compounds.Sodium
No evidence of carriage by albumin.
Sulfur
Status indeterminate for sulfur ions.
Zinc
Site A – primary,
Domain I - His67, Asn99,
Domain II - His247, Asp249.
Site II – secondary,
Subdomain IA – His9, Asp13,
Subdomain IIA - Asp255.
Site III – secondary,
Between IB and IIA domains – His157, His288 and Glu153.
Cys34 does not bind to zinc.Clinical concerns
Albumin is the primary carrier of several key physiological minerals. The evidence is extraordinarily limited regarding –
- the location of each mineral’s binding site(s),
- the factors that alter the binding site’s capacity to carry them.
Further, although some minerals are carried on the same binding site, we don’t know what determines access. In order to appropriately manage potential drug-mineral interactions, we do need to know and understand the access determinants to albumin. Essential factors include whether access is based on timing ie first come first access, or whether access is priority-based. If access is priority-based then what is the order of access, and what are the factors that alter it?
Clinical Questions
What actions will you initiate as you a review a person whose prescribed medications profile includes one or more drugs that utilize albumin as a carrier, will you -
• clarify and monitor adequacy of intake of the minerals carried by albumin that are potentially affected by their prescribed medicines?
Conclusions
Albumin and minerals in combination can have their functions impacted both directly and indirectly, by prescribed medicines.
Case study
The comments refer to the drug-nutrient, drug-food, and PharmacoNutrition effects only.
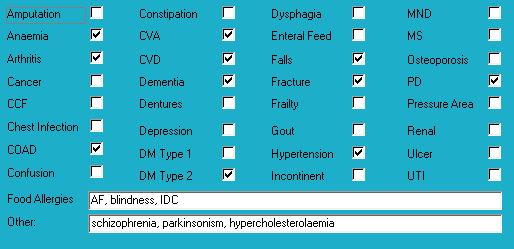
Medical history with nutritional aspect
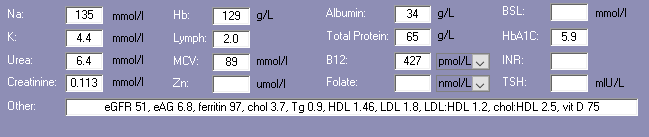
Biochemistry with nutritional aspect
Prescribed medications side effects profile - biochemistry
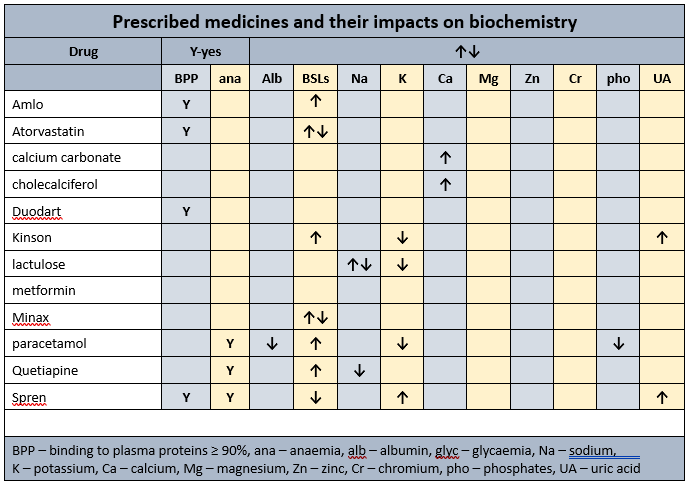
Prescribed medications side effects profile
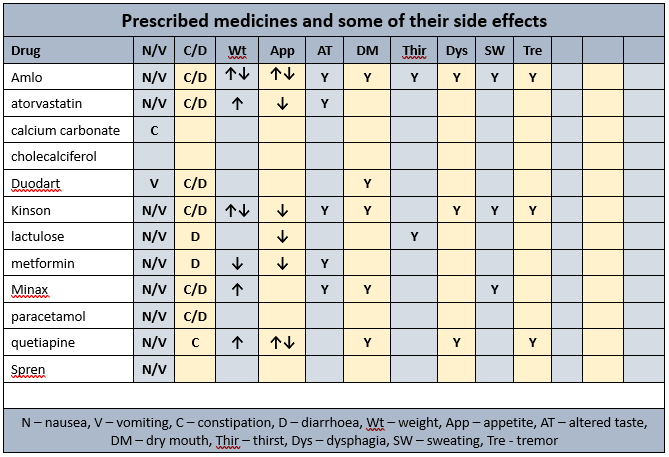
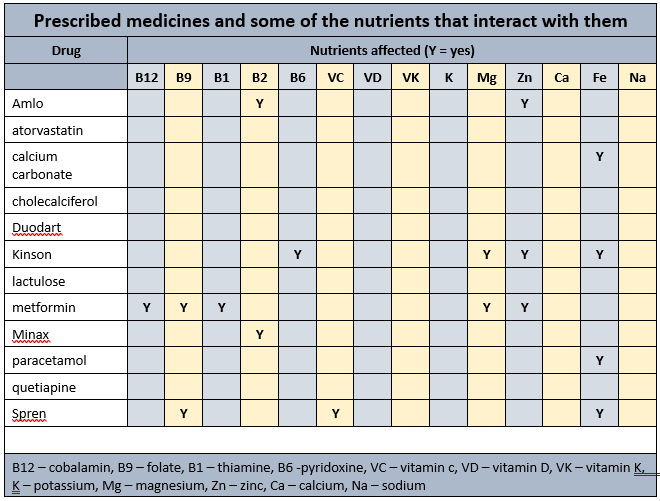
Prescribed medications affected nutrients profile
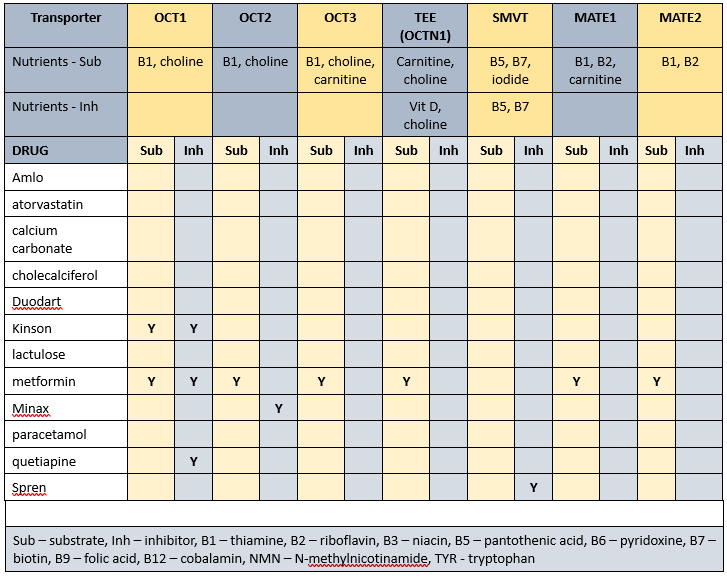
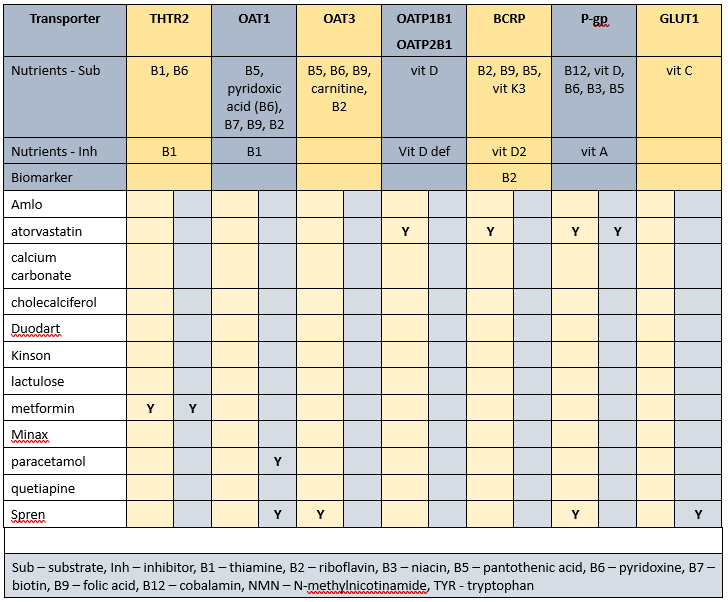
Transporter-mediated interactions and nutrients matrices
Biochemistry
Recent relevant available biochemistry indicates
- low albumin – currently prescribed paracetamol which includes hypoalbuminaemia as a side effect;
- marginal cholesterol - currently prescribed atorvastatin. There is variability between pathology laboratories with regard to appropriate lower acceptable cholesterol level - some pathology ranges have set the lower acceptable limit at 3.5, others 3.0, and some do not set a lower limit. Cholesterol is important in brain structure and function amongst many other roles.
Glycaemia
BSLs
- before breakfast - 7.3-9.4; recommended range 4-6;
- reportable limits: < 3.5 and > 15.0;
- tested daily – mane;
- last HbA1c indicates good glycaemic control.
Diabetes drugs
- novomix has a time to onset of 5-15 minutes, variable time to peak, and duration of 10-16 hours
- metformin has a duration of 12 hours
Diabetes drugs coverage
- before breakfast BSLs - minimal, if any, coverage from previous morning's novomix, nor previous evening's metformin;
- before evening meal BSLs - minimal, if any coverage from previous evening's metformin; covered by current morning's novomix and some coverage from current morning's metformin.
Mr ADN’s diabetes management includes two drugs administered before breakfast - one has a duration of about 10-16 hours and the other has a duration of about 12 hours; and one drug administered before evening meal that has a duration of about 12 hours. This means minimal drug impact on the before-breakfast glycaemia and both drugs significantly impacting late morning until late afternoon glycaemia.
Currently prescribed 7 medications that alter glycaemia.
PharmacoNutrition
Caffeine decreases effectiveness of Amlo and levodopa component of kinson.
Amlo impairs zinc status.
Caffeine increases aspirin absorption by altering gastric pH.
Vitamin C (960 mg/day) attenuates aspirin-induced gastric injury.
Aspirin inhibits vitamin C absorption by either inhibiting vitamin C binding to albumin, or by inhibiting/regulating/modulating GLUT1 (glucose transporter 1) uptake of vitamin C as DHA (dehydroascorbic acid).
If there is concurrent administration of a vitamin C intervention and aspirin then advisable to administer vitamin C prior to aspirin as vitamin C does not impact aspirin absorption whereas aspirin does negatively impact vitamin C absorption.
Aspirin has a negative impact on folate status - the mechanism of action remains speculative.
Calcium carbonate may interfere with the absorption of iron.
Coffee inhibits vitamin D uptake by inhibiting the osteoblasts (bone builders) vitamin D receptors, consequently decreasing calcium and zinc absorption
Chronic use of lactulose may promote excessive loss of water and electrolytes, especially potassium, and their regular monitoring recommended.
Levodopa component decreases zinc availability - proposed mechanism drug chelates with zinc and increases its urinary excretion.
Metformin decreases B12 absorption and decreases availability of magnesium, thiamine, vitamin C, pyridoxine and niacin. Regular monitoring B12 levels ie at least annually is now recommended.
Dietary levels of caffeine intake in conjunction with paracetamol inhibit antinocieception.
Paracetamol is a CYP1A2 substrate (can be carried by the transporter). CYP1A2 substrates include caffeine, retinol, melatonin, phosphatidylcholine, inhibitors include grapefruit juice and inducers include coffee; drug’s metabolism inhibited by caffeine therefore drug will remain active in the body for longer.
Concurrent ingestion of paracetamol and iron resulted in increased rate of iron absorption and decreased extent of absorption of paracetamol. Consequently, the authors advise different administration times from each other for the drug and iron.
There is a potential drug-nutrient interaction between kinson and calcium carbonate especially since both are prescribed for 08:00, therefore if parkinsonian control requires adjustment advisable to review administration time of calcium carbonate as a strategy to increase kinson availability and effect.
Currently prescribed vitamin D (1 tab/day). Advisable to check vitamin D levels and if still low then review current vitamin D management strategy.
Statins interfere early in the cholesterol metabolic pathway and consequently decrease -
- conversion of sun to vitamin D - vitamin D intervention recommended;
- production of CoQ10 - important in cellular energy production; CoQ10 intervention recommended;
- DHEA production - low DHEA associated with increased risk of metabolic syndrome; intervention recommended.
Prescribed medications can alter the functionality of membrane transporters and consequently the nutrients they carry. Nutrients that are affected by Mr ADN’s prescribed medications include -
- substrates – thiamine, riboflavin, niacin, pantothenate, pyridoxine, biotin, folate, B12, vitamin C, vitamin D, vitamin K3, choline, carnitine, iodide;
- inhibitors – thiamine, vitamin A, vitamin D, choline, pantothenate, biotin.
The duration of drug inhibition of transporters currently remains unknown.
Bowel management
- no regular interventions prescribed;
- oral PRN aperient prescribed;
- no Nurse Initiated interventions administered.
Staff comments
Staff advise Mr ADN is refusing to eat the minced moist diet, that he will eat mashed potatoes and pumpkin and desserts but not minced meat/fish/chicken dishes. One staff member commented that he is likely to eat very soft cutup diet as it is visually similar to the unmodified diet.
Observations
Mr ADN is a small, frail, sallow man who was sitting in the Dining Room waiting for his meal to be served - I did not interrupt as others were present at the table. He looked very unwell.
Mr ADN has remained relatively weight stable for the last year.
PharmacoNutrition comments
Mr ADN is prescribed atorvastatin which includes poor appetite in its side effect profile - it may be worthwhile considering an atorvastatin "holiday" for 3 months or until return of appetite.
Mr ADN is prescribed 7 medicines that include altered glycaemia as a side effect. Given the number of prescribed medicines that alter glycaemia, is the diagnosis of diabetes questionable, and could he actually have drug-induced hyperglycaemia? -
Chronic pain
Mr ADN’s diagnoses include chronic pain. Nutritional factors that may be useful to consider in pain management include -
- vitamin D - evidence indicates increasingly brittle pain control with decreasing/low vitamin D levels. There is increasing evidence the current minimum acceptable level for vitamin D is inadequate. Currently prescribed a vitamin D intervention;
- vitamin C - pain increases the reactive substances (formerly Reactive Oxygen Species) within cells. Vitamin C is important in quenching reactive substances and if there is insufficient vitamin C then cell status becomes compromised and the cells typically die which also causes pain. Whilst not considered part of the pain management armament, Vitamin C won't cause harm and evidence suggests it may confer benefit. Currently prescribed aspirin which decreases inhibits vitamin C access to albumin for distribution throughout the body;
- low B12 exacerbates elevated TNF- α which is an inflammatory response marker, and an elevated inflammatory response can include a pain response. Currently prescribed metformin therefore advisable to monitor B12 status on a regular basis ie at least annually;
- magnesium – proposed mechanism magnesium blocks the NMDA receptor channels in the spinal cord and thus limits the influx of calcium ie reduces the risk of excitotoxicity and consequent exacerbation of pain. Currently prescribed metformin and kinson which decrease magnesium availability.
Insulin sensitivity
Mr ADN’s diagnoses include diabetes. A number of nutritional interventions are available to improve insulin sensitivity or reduce insulin resistance including -
- vitamin D within acceptable range - evidence indicates low vitamin D is a predictor of peripheral insulin resistance and elevated inflammatory response markers. Currently prescribed a vitamin D intervention therefore advisable to monitor status early on a regular basis ie at least annually;
- magnesium – is important in glycaemic control and inadequate intake may impair insulin synthesis, secretion and signalling pathways; in fact there is evidence of an inverse correlation between magnesium status and diabetes incidence. Currently prescribed metformin and kinson which decrease magnesium availability therefore advisable to monitor status on a regular basis ie at least annually;
- thiamine - people with diabetes have a significantly increased urinary excretion of thiamine; thiamine is important in glycaemic control. Currently also prescribed metformin which decreases thiamine availability therefore advisable to monitor status on a regular basis and if levels are low then initiate an intervention;
- TNF-α – evidence indicates TNF- α has systemic effects that result in insulin resistance and NIDDM; low B12 status exacerbates elevated TNF- α. Currently prescribed metformin therefore advisable to monitor B12 status on a regular basis ie at least annually;
- zinc – is integral to insulin formation, and enhances insulin sensitivity through stimulation of insulin receptors; inadequate intake may impair insulin synthesis, secretion and signalling pathways. It is important in the glucose metabolism, protects the mitochondria from oxidative stress and glycation, and altered glomerular function, as well as modifying the inflammatory response pathway and activation of the polyol pathway (a part of intracellular signalling and metabolism). Currently prescribed amlodipine, kinson and metformin therefore advisable to clarify status and monitor on a regular basis.
Falls
Mr ADN’s diagnoses include falls. Nutritional factors that may be useful to ensure within acceptable ranges include -
vitamin D – increasing vitamin D intake increases muscle strength and decreases falls. Currently prescribed colecalciferol therefore advisable to monitor vitamin D status on a regular basis ie at least annually;
B12 - is important in the righting reflex when a person stumbles. Currently prescribed metformin therefore advisable to monitor status on a regular basis ie at least annually;
iron – currently prescribed calcium carbonate, kinson, metformin and spren therefore advisable to monitor status on a regular basis ie at least annually;
zinc – can decrease food intake through altered sense of taste and poor appetite, and consequently reduced muscle mass. Currently prescribed amlo, kinson and metformin therefore advisable to monitor status on a regular basis ie at least annually;
magnesium - magnesium is important in vitamin D activation, de novo carnitine production, and muscle function, amongst other functions. Magnesium is an intracellular ion therefore serum levels are unlikely to detect early depletion of status. Currently prescribed metformin and kinson which decrease magnesium availability therefore advisable to monitor status on a regular basis ie at least annually;
thiamine –is important in balance and position sense Currently also prescribed metformin which decreases thiamine availability therefore advisable to monitor status on a regular basis and if levels are low then initiate an intervention.
Dysfunctional mitochondria
Mitochondrial dysfunction is now being linked to a number of disorders including heart failure, cardiovascular diseases, diabetes, neurodegenerative diseases (MS, Huntingtons, Parkinsons, MND, Alzheimers, glaucoma), ageing, mitochondrial diseases, retinis pigmentosa, CVA, epilepsy, cardiomyopathy, autism, muscular dystrophy, atypical learning disabilities, fibromyalgia, Chronic Fatigue Syndrome, Developmental Delay, Cerebral Palsy, bipolar disorder, major depression disorder, schizophrenia, pulmonary fibrosis, obesity and likely others. Several of MrADN's diagnoses fall within this umbrella
The primary function of mitochondria is the generation of ATP (energy). Whilst the nutritional contribution to neurodegenerative disorders and mitochondrial dysfunction is still in the early stages of research, it is likely nutritional interventions won’t cause harm and will probably confer benefit. Nutrients that support dysfunctional mitochondria include -
- Magnesium – important in the electron transport chain (etc) and oxidative phosphorylation. Currently prescribed metformin and kinson which decrease magnesium availability therefore advisable to monitor status on a regular basis ie at least annually;
- Thiamine – deficiency impairs oxidative phosphorylation. Currently prescribed metformin which decreases thiamine availability therefore advisable to monitor status on a regular basis and if levels are low then initiate an intervention;
- zinc – protects the mitochondria from oxidative stress and glycation, and altered glomerular function, as well as modifying the inflammatory response pathway and activation of the polyol pathway (a part of intracellular signalling and metabolism). Currently prescribed amlo, kinson and metformin therefore advisable to monitor status on a regular basis ie at least annually.
What else would you include?
Please read this as it is important …
The information in this article is provided to support Health Professionals. It is not an exhaustive protocol and Health Professionals are advised that adequate professional supervision is accessed to ensure that Duty of Care obligations with respect to safe administration of medicines is met for each consumer.

