
Mechanisms and consequences
Albumin aka Human Serum Albumin (HSA) is the main protein in the blood. It is part of a superfamily that includes vitamin D-binding protein (VDP), alpha-fetoprotein and alpha-albumin (afamin). Recent seminal research (DOI https://doi.org/10.1186/s12967-024-05000-5) has also identified albumin as a glycoprotein.
Because albumin is their primary distribution carrier, how compounds interact with albumin determines compound half-life, absorption, distribution, metabolism, and excretion.
Both albumin and the membrane transporters are commonly referred to as transporters. To minimise confusion, I shall refer to blood-specific distribution vehicles as carriers.
Functions
Albumin’s range of functions is extensive and includes -
- modulator of plasma oncotic pressure (the pressure exerted by plasma proteins on capillary walls), osmotic pressure, and pH;
- endothelial stabilization, immune regulation, enzyme activities, and anti-oxidant properties;
- carrier of endogenous compounds including water, bilirubin, fatty acids, nutrients;
- carrier of exogenous compounds including metals, toxins, pharmaceuticals;
- biomarker of oxidative stress;
- biomarker of diseases such as cancer, rheumatoid arthritis, diabetes;
- biomarker of a person's nutritional status, and a predictor of the outcome of many pathologies.
In some disease states, albumin can -
- be reduced in quantity and quality. The concept of ‘effective albumin concentration” refers to the amount of albumin that is structurally and functionally intact;
- have normal quantity, and altered function;
- be sufficiently modified that its binding properties and function are significantly affected to alter physiological responses.
Synthesis
- typically takes about 15-30 minutes to produce,
- rate of synthesis that depends on amino acid supply, especially tryptophan, and is also affected by nutritional status and oncotic pressure,
- circulatory half-life is 16 hours,
- continuous secretion into the bloodstream,
- healthy adults produce 10–15 g of albumin per day,
- typical healthy adult range is 35‑50 g/L.
Hypoalbuminaemia
Hypoalbuminaemia occurs when there is both reduced synthesis and increased catabolism.
Factors causing hypoalbuminaemia include fasting, poor nutritional status, high osmotic pressure, and inflammation eg tumor necrosis factor α (TNFα), interleukin‑6 (IL-6).
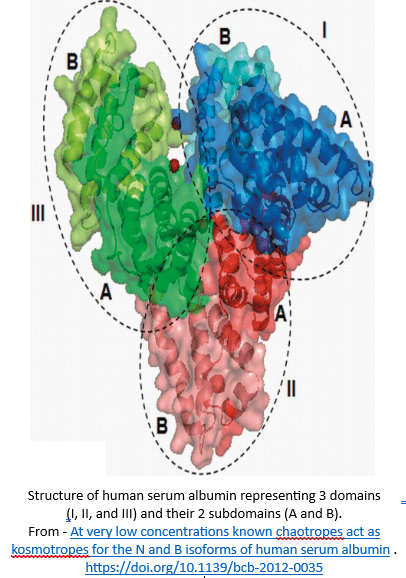
Albumin structure
The albumin structure is a single chain polypeptide (amino acids) chain. It comprises 3 domains (I, II, III), and each domain contains 2 subdomains (A, B). There is minimal contact between domains I + III, and all primary contact is through domain II. The subdomains contain a variety of amino acid-based binding sites.
The structure is very open and vaguely based on a heart or V shape. The open structure means it can carry compounds with a variety of shapes and sizes. A range of factors, endogenous and/or exogenous, can alter albumin’s structure, resulting in altered functionality and effectiveness. The ultimate outcomes of modification to albumin’s structure are both altered metabolic processes, and altered therapeutic benefit of interventions.
Some analogies about albumin. Albumin has size constraints like a cargo plane and cannot add extra trailers like a road train. It has defined zoned areas with limited overlap like a cargo boat (wheelhouse, kitchen/galley, crew quarters, engine room, cargo). Its route is defined similarly to a train.
Binding sites
The albumin structure is designed to accommodate multiple binding sites and with some flexibility for compound shape and size.
Binding between compounds and albumin is determined by the number and availability of binding sites for each compound, and albumin’s affinity for the compound.
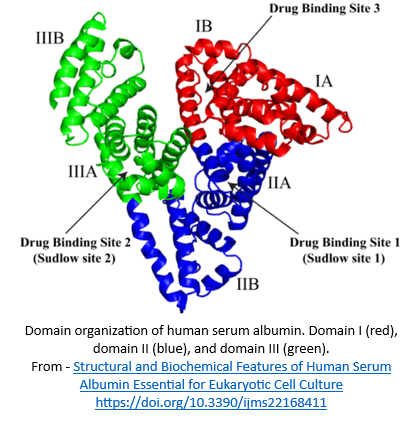
Identified binding sites include -
- Sudlow site I. Aka FA7 (Fatty Acid) site, and is located in subdomain IIA. Compounds include bulky heterocyclic molecules such as dicarboxylic acids. Site I shows poor stereoselectivity, which might also be due to the flexibility of this site.
- Sudlow site II. Aka FA3-4 site, and is located in subdomain IIIA. Compounds include aromatic carboxylates with an extended conformation. Site II often shows stereoselectivity and therefore is less flexible.
- Binding site 3. Aka FA1 site and is located in subdomain IB.
- FA5 site. Located in subdomain IIIB.
- Subdomains IA + IIB. The evidence is sparse to non-existent with regard to any compounds associated with these subdomains.
There seem to be 3 key areas for albumin-based drug-nutrient interactions –
- structural changes altering access to binding sites, especially nutrient access. Note - drug-induced structural changes impacting drug effects are much more likely to be investigated and known;
- competition between drugs and nutrients for shared binding sites;
- inhibited access to the carrier. A known example is aspirin’s inhibition of vitamin C access to albumin (MedNut Mail Aspirin-vitamin C interactions).
I have allocated these mostly unknown, key interactions to the “why don’t we know this already” basket.
Clinical concerns
The “salting” of drugs with nutrients to utilise albumin as their distribution vehicle is a potential source of nutrient toxicity. Consequently, nutrient content in each drug dose should be included in the Product Information documents. As these are “new” techniques, the Regulators are yet to initiate any decrees – let’s hope they do so and soon.
There is no regulatory requirement for Product Information documents to include –
- the impacts of pharmaceuticals and nutrients the albumin structure,
- the specific subdomains and their specific binding sites for each pharmaceutical product.
Clinical Questions
What actions will you initiate as you a review a person whose prescribed medications profile includes one or more drugs that utilize albumin as a carrier, will you -
- recommend checking inflammatory markers such as TNF-α and IL-6, and B12 status (because it also impacts TNF-α status) if hypoalbuminaemic?
Conclusions
Albumin is the primary carrier in the body’s distribution system. The evidence for albumin-based drug-nutrient interactions is remarkably limited.
Case study
The comments refer to the drug-nutrient, drug-food, and PharmacoNutrition effects only.
Data summary
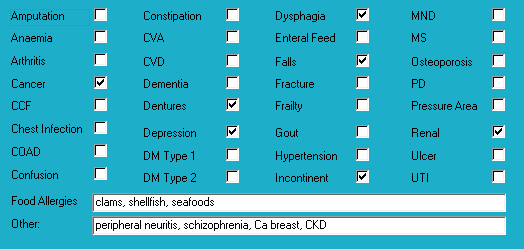
Medical history with nutritional aspect
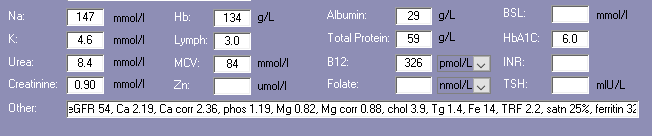
Biochemistry with nutritional aspect
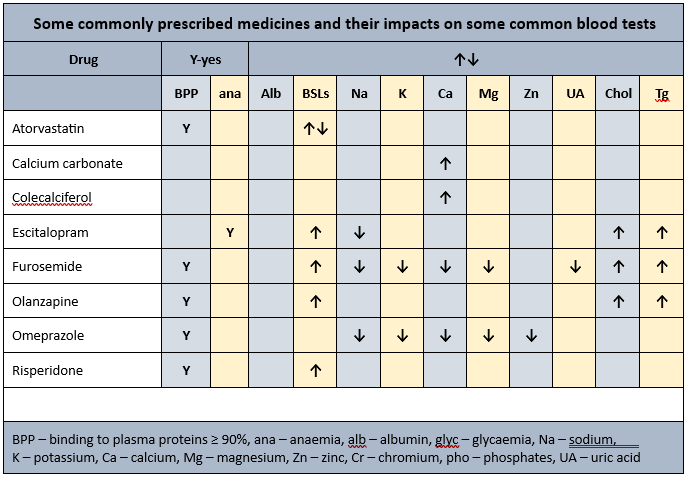
Prescribed medications side effects profile - biochemistry
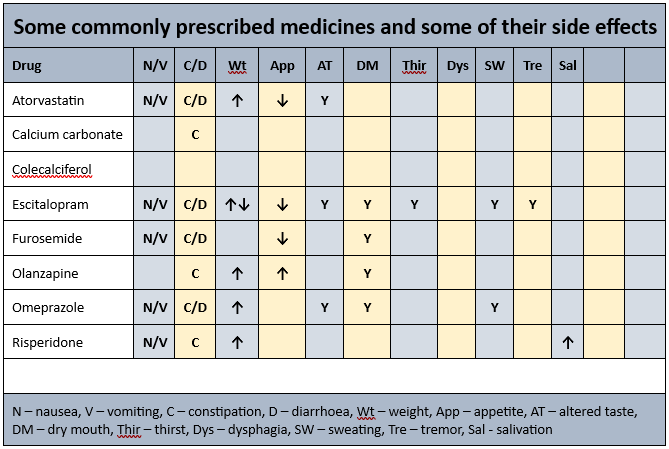
Prescribed medications side effects profile
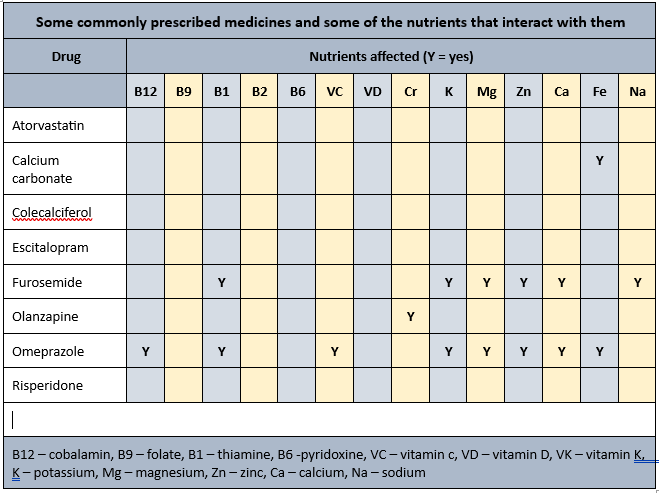
Prescribed medications affected nutrients profile
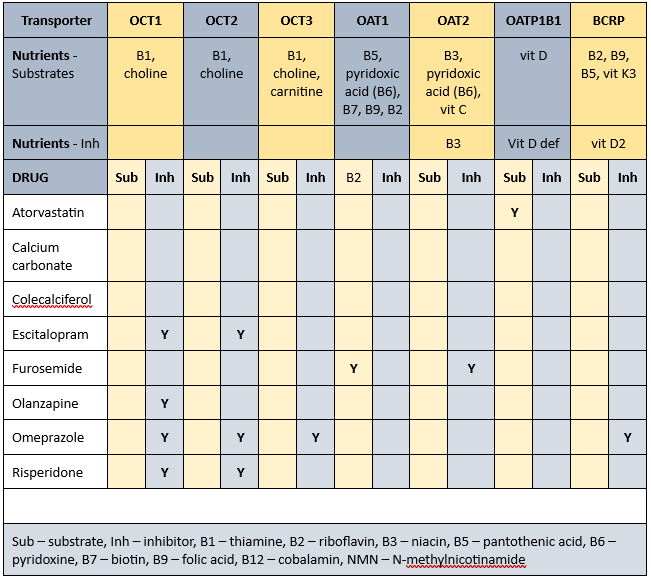
Transporter-mediated interactions and nutrients matrix
Biochemistry
Old" biochemistry indicates low albumin + total proteins - The plasma proteins are the primary transporters for 4 of the prescribed drugs and hypoalbuminaemia may alter their effects.
Glycaemia
Currently prescribed 5 medications that alter glycaemia.
Pharmaconutrition
Calcium carbonate may interfere with the absorption of iron, therefore advisable to continue to monitor iron status.
Cholecalciferol (2000 IU/day) has been prescribed since admission therefore advisable to clarify current status as evidence indicates this level of intervention is adequate to maintain current status.
Coffee inhibits vitamin D uptake by osteoblasts (bone builders) by inhibiting their vitamin D receptors, and consequently decrease calcium and zinc absorption and currently prescribed a vitamin D intervention therefore advisable to clarify status.
Frusemide increases urinary excretion of calcium, magnesium, potassium, sodium and thiamine.
Olanzapine is a CYP1A2 substrate (can be carried by the transporter). CYP1A2 substrates include caffeine, retinol, melatonin, phosphatidylcholine, inhibitors include grapefruit juice and inducers include coffee; drug’s metabolism inhibited by caffeine therefore drug will remain active in the body for longer.
Omeprazole decreases B12, vitamin C, magnesium, zinc and iron absorption, may decrease calcium absorption, and decreases thiamine availability.
Advisable to clarify why calcium carbonate is prescribed. Calcium carbonate requires gastric acidity for absorption however omeprazole prescribed and therefore minimal calcium absorption. Advisable to consider calcium citrate which does not require gastric acidity for absorption.
Currently prescribed the daily double ie two drugs decrease magnesium availability - being furosemide and omeprazole. Magnesium deficiency manifests as confusion, disorientation, personality changes, loss of appetite, depression, muscle cramps, tingling, numbness, hypertension, cardiac dysrhythmia, seizures. Magnesium is an intracellular ion therefore serum levels are unlikely to detect early depletion of status. Cellular magnesium status remains unknown whilst magnesium levels within acceptable range however if magnesium levels are low then that typically indicates significant cellular depletion and intervention recommended. Further, magnesium is important for the activation of thiamine, vitamin C, vitamin D, iodide and the de novo synthesis of carnitine. Advisable to monitor status on a regular basis whilst furosemide and/or omeprazole prescribed.
Statins interfere early in the cholesterol metabolic pathway and consequently decrease -
- conversion of sun to vitamin D - vitamin D intervention recommended;
- production of CoQ10 - important in cellular energy production; CoQ10 intervention recommended;
- DHEA production - low DHEA associated with increased risk of metabolic syndrome; intervention recommended.
Advisable to check lipid levels and if within acceptable range then review necessity for atorvastatin’s continued prescription. There is variability between pathology laboratories with regard to appropriate lower acceptable cholesterol level - some pathology ranges have set the lower acceptable limit at 3.5, others 3.0, and some do not set a lower limit.
Membrane transporters
Some of the identified membrane transporters alter the absorption and/or organ and cellular uptake of a range of nutrients. Inhibition of membrane transporters means blood test results may be unreliable. To clarify nutrient status advisable to conduct blood tests at least one hour before administration of relevant prescribed medicines. A concurrent detailed Diet History is also essential to corroborate adequacy of intake of all affected nutrients. Further, all affected nutrients to be monitored on a regular basis ie at least annually.
Nutrients that are affected by Mrs ADK’s prescribed medications include -
- substrates – thiamine, riboflavin, niacin, pantothenate, pyridoxine, biotin, folate, vitamin C, vitamin D, vitamin K3, choline, carnitine;
- inhibitors – niacin, vitamin D def, vitamin D2.
The duration of drug inhibition of transporters currently remains unknown.
Bowel management
- regular intervention prescribed - no,
- PRN interventions prescribed - no,
- Nurse Initiated interventions administered - no.
Staff comments
Staff advise Mrs ADK mostly does not eat breakfast, usually eats a good midday meal, and eats well at the evening meal; she does not like desserts. They also commented Mrs ADK is a smoker, "likes a drink", and is often up and about until quite late; and suggested she may benefit from a grazing plate if weight status is a concern.
I was unable to locate Mrs ADK to have a chat.
Mrs ADK seems to have been losing weight in recent times.
PharmacoNutrition comments
Mrs ADK has seemingly has had a loss of weight of 5 kg in one month in the presence of good appetite, albeit not eating desserts – she is currently prescribed 3 drugs that decrease appetite and only one that increases appetite. Dessert refusal may indicate altered sense of taste, and given the combination of weight loss and prescription of omeprazole and furosemide, advisable to check zinc level. Zinc is important in the sense of taste and release of the hunger hormone Neuropeptide Y.
PPI prescription
Mrs ADK has been prescribed a proton pump inhibitor since admission ie 11 years ago. Increasing evidence that longterm (3+ years) proton pump inhibitor prescription is associated with -
- increased risk of food sensitivities at a level of peanut allergy, due to partial protein digestion;
- increased risk of coeliac disease due to partial protein digestion;
- altered gut microbiome;
- increased risk of scurvy;
- generalised malnutrition due to impaired absorption of a range of nutrients such as B12, vitamin C, magnesium, zinc, iron, etc;
- altered gastric pH which reduces absorption dynamics of a range of drugs and nutrients. Altered drug availability is relatively easily identified however reduced nutrient absorption is rarely identified due to the non-specific nature of their signs and symptoms.
Consequently, advisable to reconsider reviewing current proton pump inhibitor prescription and consider -
- whether proton pump inhibitor prescription is still required,
- if suppression of gastric acidity is still required then could it be managed with an H2 antagonist such as ranitidine (there is a general belief that they cause less nutritional harm than proton pump inhibitors).
Calcium carbonate requires gastric acid for absorption however proton pump inhibitors such as omeprazole reduce gastric acid availability and therefore decrease calcium absorption. Calcium citrate preferred option as a calcium supplement as gastric acid not required for its absorption.
Drug-induced hyperglycaemia
Mrs ADK is at risk of a diagnosis of diabetes as she is prescribed 5 medicines that include altered glycaemia as a side effect. It is likely the hyperglycaemia will resolve upon cessation of the relevant medicines, and unlikely she has developed a metabolic disorder. Further, management strategies for drug-induced hyperglycaemia may differ from those for diabetes-induced hyperglycaemia, likely mechanisms of action include -
- Thiamine. Important in carbohydrate metabolism. Currently prescribed furosemide and omeprazole therefore advisable to clarify thiamine status and if low then intervention recommended;
- Vitamin C. Has been found to confer beneficial impacts on HbA1c and fasting glucose and insulin levels. Currently prescribed omeprazole therefore advisable to clarify vitamin C status and if low then intervention recommended;
- Calcium. Is important in insulin production. Currently prescribed furosemide and omeprazole therefore advisable to clarify calcium status and if low then intervention recommended;
- Chromium. Enhances the effectiveness of insulin. Chromium status influenced by iron status as they share the same carrier. Currently prescribed olanzapine therefore advisable to clarify chromium status and if low then intervention recommended;
- Iron. The beta cells in the pancreas do not tolerate inadequate or excessive iron intake and decrease insulin production as a consequence. Currently prescribed calcium carbonate and omeprazole therefore advisable to clarify iron and copper levels and initiate an intervention if either are low;
- Magnesium. Is important for activation of thiamine, vitamin C and vitamin D, and regulation of the IR/IRS/PI3K/PDK/Akt/GLUT4 pathway. Currently prescribed furosemide and omeprazole therefore advisable to clarify vitamin D status and if low then intervention recommended.
Falls
Mrs ADK’s diagnoses include falls. Nutritional factors that may be useful to ensure within acceptable ranges include –
potassium - important in muscle function, currently prescribed furosemide and omeprazole therefore advisable to clarify status;
calcium - more likely to be low if potassium or magnesium low; important in muscle function, currently prescribed furosemide and omeprazole therefore advisable to clarify status;
B12 - is important in the righting reflex when a person stumbles; prescribed omeprazole therefore advisable to check status;
zinc – can decrease food intake through altered sense of taste and poor appetite, and consequently reduced muscle mass; currently prescribed furosemide and omeprazole therefore advisable to monitor status;
magnesium - magnesium is important in vitamin D activation, de novo carnitine production, and muscle function, amongst other functions. Also currently prescribed furosemide and omeprazole which significantly decreases magnesium availability. Advisable to clarify magnesium status;
thiamine –is important in balance and position sense. Currently prescribed furosemide and omeprazole therefore advisable to monitor status.
What else would you include?
Please read this as it is important …
The information in this article is provided to support Health Professionals. It is not an exhaustive protocol and Health Professionals are advised that adequate professional supervision is accessed to ensure that Duty of Care obligations with respect to safe administration of medicines is met for each consumer.

