
Mechanisms and consequences
The body’s distribution system comprises a framework of local transporters, hubs, and systemic carriers. We see examples of this framework in operation in our social structures such as -
- the Postal Service. Designated sorting centres distribute to local hubs that then distribute by electric bike, truck etc, to the final destination;
- the suburban + interstate rail and bus networks. Trains and buses move travellers to centralised hubs where they connect with other (interstate) rail or bus system;
- the niche + national airline carriers. Similar concept to the rail and bus networks;
- the grain harvest network. Local trucks move grain to railhead silos, then grain trains move it to ports, and then ships move it to its next destination.
Distribution system in the body
Essentially, local shuttle buses collect their load and move it to a departure point. At the departure point the load is transferred to a systemic carrier and moved to its destination. Upon arrival, a local shuttle bus then moves it to its point of operation.
Our knowledge of how the distribution system actually functions falls into 2 broad categories, being –
- the stuff we know – a very small category,
- the stuff we don’t know – a very, very, large category.
The stuff we know
Transporters. The shuttle buses aka the local delivery service. Approximately 9 transporters are required to be tested for and identified in the drug discovery process and Product Information documents. Although known, some are not required to be tested for and identified in the drug discovery process and Product Information documents eg glucose transporters. The vast majority are unknown and euphemistically referred to as “passive diffusion”.
Carriers. The systemic carriers that typically move load from a departure point to an arrivals point, for local distribution. The main carrier is albumin, followed by alpha-1 acid glycoprotein, and then several niche carriers.
The stuff we don’t know
The logistics of how it all functions. How does the load find the relevant transporter? Do the transporters wait for the load, or does the load wait somewhere until the transporter arrives? Does the load accumulate somewhere until a carrier arrives, or do the carriers wait for the load? Is there a designated “arrivals lounge” equivalent where the load waits until the relevant transporter arrives?
When aspirin inhibits vitamin C boarding the albumin carrier, what does the vitamin C then do? Does it wait until aspirin’s inhibition wears off, and then board the next available albumin? Or does it hop on a transporter back to the gut and be excreted?
If there is more load than capacity, what determines which waiting loads are, and are not, included?
Different substances can modify albumin’s structure and therefore function, and consequently also influences what it carries. It seems likely various substances have similar effects on other carriers.
Nutritional consequences
What are the nutritional consequences of impairment to the distribution system? What determines which compound is preferentially selected when there is competition for the available transfer capacity? And what happens to the compound that is not selected?
How can we ascertain whether anomalies between food intake and blood test results are due to interferences in the distribution system?
Because we don’t have a very clear understanding of how the body’s distribution system functions, we are not aware of potential drug-distributor interactions that may also be negatively impacting our nutritional health.
Clinical concerns
Given all pharmaceuticals utilise the body’s distribution system, and the research seems to be very limited, we are likely working with drug-nutrient interactions within the system already. We need –
1. regulatory requirement that drug impacts on all aspects of the body’s distribution system be included in the drug discovery process and included in the Product Information documentation;
2. a concerted research program to identify the negative impacts of alteration to the distribution system on nutritional factors;
3. a concerted research program to identify strategies to ensure nutrient “preference for transfer” by the distribution system, to minimise exogenous negative impacts.
Clinical Questions
What actions will you initiate as you a review a person’s prescribed medications, will you -
- consider opportunities to increase nutrient uptake as a strategy to offset impairment to the distribution system?
Conclusions
The distribution system is a likely source of a range of potential drug-nutrient interactions that are currently unknown.
Case study
The comments refer to the drug-nutrient, drug-food, and PharmacoNutrition effects only.
Data summary
Medical history with nutritional aspect
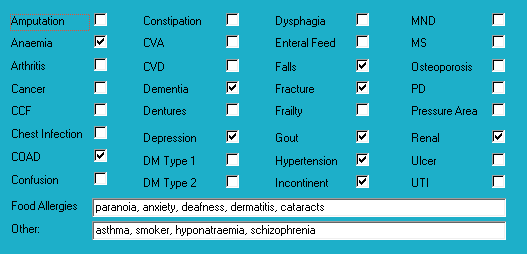
Medical history also includes - chronic alcoholism, vision-impaired.
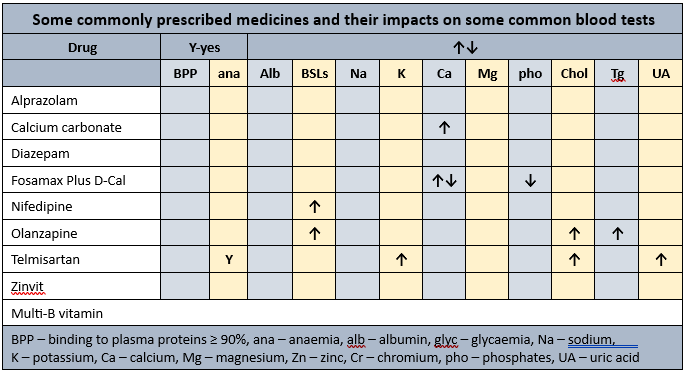
Biochemistry with nutritional aspect
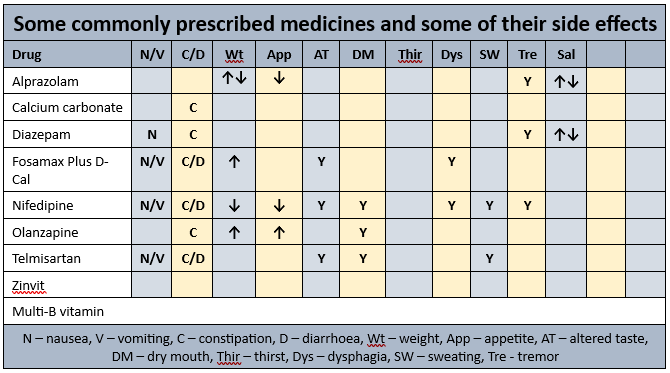
Prescribed medications side effects profile
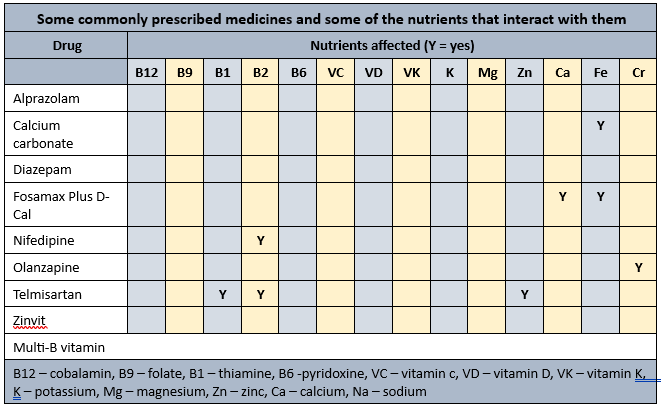
Prescribed medications affected nutrients profile
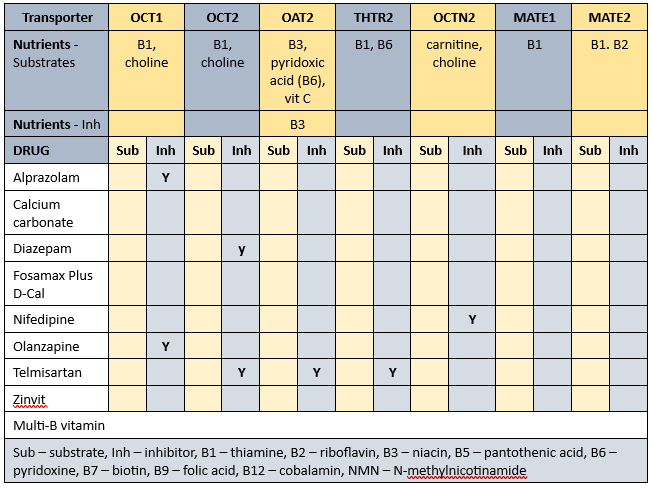
Transporter-mediated interactions and nutrients matrix
Biochemistry
Relatively recent available biochemistry indicates -
- low zinc - commenced zinvit 4 months ago. Advisable to check status and if within acceptable range then cease the intervention. However, given telmisartan is prescribed, advisable to monitor zinc status on a regular basis to ensure it does not fall below acceptable range again;
- elevated CRP+ESR - inflammatory response markers; associated with increased resting metabolic rate and consequent increase in energy (food) requirements; influenced by vitamin D status and currently prescribed a vitamin D intervention.
Advisable to check plasma proteins (albumin, total proteins) as markers of nutritional status. The plasma proteins are the primary transporters for 4 of the prescribed drugs and hypoproteinaemia may alter their effects.
Glycaemia
Currently prescribed 2 medications that cause hyperglycaemia.
Pharmaconutrition
Calcium carbonate may interfere with the absorption of iron therefore advisable to monitor iron status on a regular basis.
Early evidence found olanzapine both negatively affects chromium accumulation and increases chromium excretion ie resulting in nett chromium loss. Chromium intervention advisable as chromium is rapidly lost from the body, and is important in glycaemic control.
Telmisartan is likely to reduce zinc status and currently prescribed a zinc intervention.
Alendronate plus vitamin D typically provide about 140 mcg vitamin D per week; 1000 IU vit D/day provides about 175 mcg vit D/week. Advisable to check vitamin D levels and if still low then review current vitamin D management strategy and consider an alternative, more effective product.
Membrane transporters
Some of the identified membrane transporters alter the absorption and/or organ and cellular uptake of a range of nutrients. Inhibition of membrane transporters means blood test results may be unreliable. To clarify nutrient status advisable to conduct blood tests at least one hour before administration of relevant prescribed medicines. A concurrent detailed Diet History is also essential to corroborate adequacy of intake of all affected nutrients. Further, all affected nutrients to be monitored on a regular basis ie at least annually.
Nutrients that are affected by Mrs ADJ’s prescribed medications include -
- substrates – thiamine, niacin, pyridoxine, carnitine, choline, vitamin C;
- inhibitors – niacin.
The duration of drug inhibition of transporters currently remains unknown.
Bowel management
- no regular intervention prescribed;
- oral PRN aperients prescribed;
- no Nurse Initiated interventions administered.
Staff comments
Staff advise Mrs ADJ eats most of her food most of the time.
Observations
Mrs ADJ is a small, elegant lady with a large abdo and who was sitting in the lobby when I went to speak to her - she told me she eats well, sleeps well, does not feel upset in the tummy, and wouldn't answer any more of my questions.
Mrs ADJ 's weight has fluctuated from admission, with an overall downward trend - likely cause being reduction in alcohol intake. Mrs ADJ has lost weight recently, and has been weight stable about 47 kg for the last 4 months.
Pharmaconutrition comments
Many of Mrs ADJ 's diagnoses fit within the metabolic syndrome cluster. There are a number of nutritional interventions to improve insulin sensitivity or reduce insulin resistance including -
- vitamin D within acceptable range - current intervention may not be adequate to attain adequate range. Early evidence indicates low vitamin D is a predictor of peripheral insulin resistance and elevated inflammatory response markers;
- magnesium – is important in a range of metabolic processes - advisable to review status;
- chromium - evidence indicates chromium both increases the number of insulin receptor cells on cell walls, and improves intracellular response to insulin th;refore intervention advisable.
- thiamine - people with diabetes have a significantly increased urinary excretion of thiamine; thiamine is important in glycaemic control. Advisable to monitor thiamine status;
- biotin – evidence indicates biotin is important in a number of steps in carbohydrate metabolism. Advisable to monitor status;
- TNF-α – evidence indicates TNF- α has systemic effects that result in insulin resistance and NIDDM; low B12 status exacerbates elevated TNF- α therefore advisable to check B12 status;
- zinc – protects the mitochondria from oxidative stress and glycation, and altered glomerular function, as well as modifying the inflammatory response pathway and activation of the polyol pathway (a part of intracellular signalling and metabolism). Currently prescribed a zinc intervention and ongoing telmisartan which depletes zinc status therefore advisable to monitor status regularly.
Falls
Mrs ADJ’s diagnoses include falls. Nutritional factors that may be useful to ensure within acceptable ranges include –
iron – important in balance and currently prescribed calcium carbonate therefore advisable to check status;
zinc – can decrease food intake through altered sense of taste and poor appetite, and consequently reduced muscle mass. Currently prescribed telmisartan and a zinc intervention therefore advisable to monitor status;
thiamine –is important in balance and position sense. Currently prescribed telmisartan therefore advisable to monitor status.
Deafness
Mrs ADJ’s diagnoses include deafness. Nutritional factors to ensure within acceptable ranges include –
zinc - inadequate zinc status has been associated with impaired hearing. Currently prescribed telmisartan and a zinc intervention therefore advisable to monitor zinc status;
thiamine – associated with bilateral hearing loss and proposed mechanism of action is that thiamine transporter OCT2 is expressed in the hair cells of the cochlea therefore interruptions to thiamine accessibility are likely to impact hair cell function. Currently prescribed telmisartan and a B-vitamin intervention therefore advisable to monitor thiamine status on a regular basis.
What else would you include?
Please read this as it is important …
The information in this article is provided to support Health Professionals. It is not an exhaustive protocol and Health Professionals are advised that adequate professional supervision is accessed to ensure that Duty of Care obligations with respect to safe administration of medicines is met for each consumer.

