
Drug-induced hypoalbuminaemia (low albumin) is a multifaceted issue that impacts physiological function both directly and indirectly. Albumin is the primary carrier in the blood of many vitamins, minerals and other substances including many commonly prescribed medicines.
Hypoalbuminaemia occurs as a consequence of -
- decreased albumin production,
- inadequate protein intake,
- increased albumin excretion.
Nutritional causes of hypoalbuminaemia
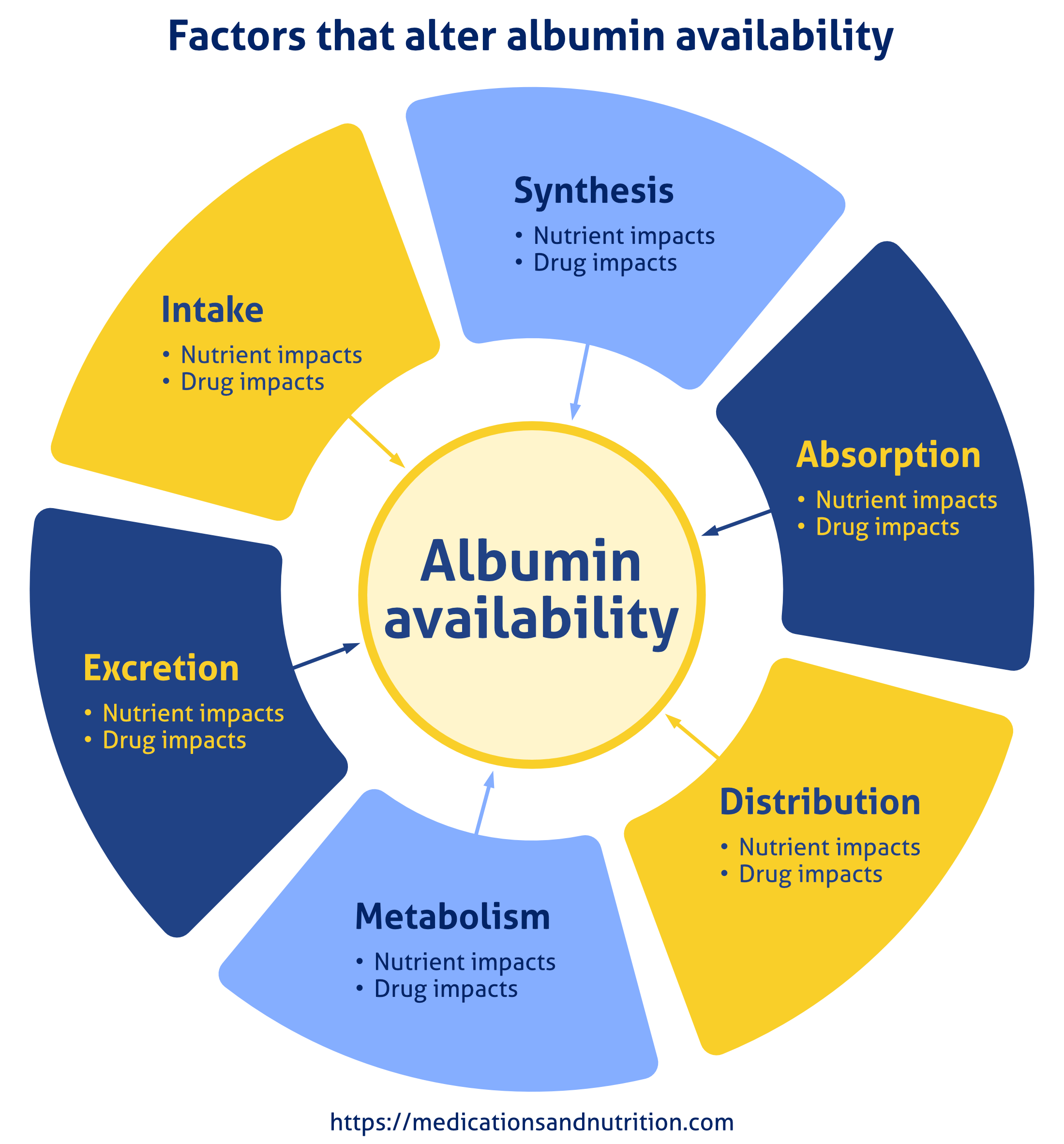
Nutritional causes of hypoalbuminaemia encompass synthesis (production), intake, absorption, distribution, metabolism and excretion.
1. Reduced albumin synthesis
Albumin is produced in the liver, therefore damage to the liver can limit albumin production. Synthesis requires adequate supply and availability of nutrients, amino acids and energy (kilojoules/calories).
Drug impacts can cause impairment to liver function with mechanisms of action including -
- reduced amino acid availability – decreasing appetite and/or other side effects that negatively impact food intake. For example, paracetamol metabolism increases the demand for the amino acid cysteine;
- likely reduced nutrient availability eg proton pump inhibitors (PPIs) decrease availability of vitamin C, magnesium, zinc, and others;
- likely inhibition of some of the transporters that provide amino acids to the liver.
2. Reduced intake
Factors that influence dietary choices include -
- disease impacts eg anaemia;
- disease-induced dietary restrictions eg coeliac, food sensitivities;
- daily food choices eg fad diets;
- social factors such as financial pressures, shopping difficulties, housebound, grieving;
- mechanical factors such as the ability to -
- move food from plate to mouth eg tremor, dementia;
- chew and swallow safely eg ill-fitting dentures typically due to weight change;
- dine in a conducive environment eg noisy, unlooped, dining environments fill hearing aids with noise;
- see the meal eg unaware the meal is served or the meal’s composition;
- eat enough to meet energy requirements eg the dementia “walking all day” stage.
Drug impacts can reduce food intake by -
1. Side effects profile -
- directly – decreasing appetite;
- indirectly - nausea, vomiting, constipation, diarrhoea, altered taste, dry mouth, tremor, tardive dyskinesia, impaired hearing, impaired vision, etc;
2. Ingredient (excipient) content eg many drugs include gluten, lactose, etc.
3. Decreased nutrient absorption
Factors that influence nutrient absorption include -
1. Digestive tract pH – altered pH changes nutrient availability and absorption;
2. Transporter availability - moves nutrients from intestines, cells and the kidneys to the blood for distribution;
3. Carrier availability - moves the substances in the blood to their cellular destinations.
Drug impacts can decrease nutrient absorption by -
- altering gastric pH - eg proton pump inhibitors change gastric pH thus impairing/inhibiting absorption of iron, magnesium, zinc, etc;
- occupying or inhibiting transporters eg metformin occupies (is a substrate for) THTR2 (Thiamine Transporter 2) which transports thiamine. Fedratinib inhibits (blocks transporter function) OCT2 (Organic Cation Transporter 2) which is a thiamine and choline transporter.
4. Altered nutrient distribution
Factors that influence nutrient distribution include availability of -
- membrane transporters – their occupation or inhibition can alter nutrient availability;
- blood carriers – enough carriers to meet load demand when required;
Drug impacts can alter nutrient distribution by –
- Membrane transporters – eg fedratinib is both a substrate and inhibitor for transporter P-glycoprotein (P-gp). P-gp substrates include pyridoxine, nicotinamide, pantothenate, cobalamin and vitamin D, and P-gp inhibitors include vitamin A;
- Carriers – eg ibuprofen binding to albumin prevents zinc binding to its MBS-A site and therefore decreases activated insulin availability.
5. Altered metabolism
Factors that influence metabolism include -
1. Thyroid status – altered thyroid status means altered energy requirements and utilization;
2. Activity and exercise – increase energy consumption and rate of utilization, therefore increase energy intake requirements;
3. Key nutrient availability – influences which metabolic pathways are available. For example, riboflavin (B2) is essential for pyridoxine (B6) activation which is essential for niacin (B3) activation which is essential for oxidative phosphorylation to proceed. Inadequate B2 availability means a change in energy metabolic pathways from oxidative phosphorylation to aerobic glycolysis.
Drug impacts to metabolism include -
- thyroid function – eg drugs such as citalopram, lurasidone, quetiapine include hypothyroidism in their side effects profile;
- the metabolic rate - eg propranolol increases rate and thyroxine decreases rate;
- metabolic pathways - eg metformin decreases riboflavin availability.
6. Increased nutrient excretion
Factors that influence nutrient excretion include transporter availability to move nutrients into and out of the kidneys.
Drug impacts on nutrient excretion include inhibition of renal transporters - eg cetirizine is an OCT2 inhibitor, OCT2 substrates include choline and thiamine.
Consequences of hypoalbuminaemia
Inadequate optimal nutrient intake means insufficient tools available for the liver to produce adequate albumin.
Because there are fewer binding sites for substrates such as drugs, their unbound levels increase thus increasing drug dose availability. Increasing drug dose may or may not be desirable as there is an increased risk of toxicity.
Reduced availability of binding sites on albumin means reduced levels of activated insulin.
Ultimately hypoalbuminaemia alters both nutrient and drug availability.
Clinical concerns
Trying to identify the mechanisms of action that specific drugs utilise to cause hypoalbuminaemia is like trying to nail water.
Understanding the interrelationships between the trifecta of disease, nutrition and polypharmacy is essential for optimizing therapeutic outcomes. We particularly need to understand the trifecta’s impacts –
- on the transfer of vitamins, minerals and other substances across membranes;
- on plasma concentrations of relevant nutrients and other substances and those consequences.
Factoring the consequences of albumin’s functional and allosteric linking into our clinical management is not a commonly acknowledged issue in nutrition management therefore few, if any, tested management strategies have been developed.
Clinical Questions
When you review a person’s prescribed medicines that include hypoalbuminaemia as a side effect, and the person has hypoalbuminaemia, would you -
Conclusions
Drug-induced hypoalbuminaemia is a multifaceted issue that profoundly alters nutritional health and the therapeutic benefits of prescribed medicines.
Please read this as it is important …
The information in this article is provided to support Health Professionals. It is not an exhaustive protocol and Health Professionals are advised that adequate professional supervision is accessed to ensure that Duty of Care obligations with respect to safe administration of medicines is met for each consumer.

